Infertility is brought on by sperm in roughly 50% of infertile couples. The most popular and effective treatment for male infertility is ICSI. Here’s who ICSI might be suitable for and what the risks are.
What is ICSI?
Intracytoplasmic sperm injection (ICSI) has gradually replaced traditional IVF and other forms of micromanipulation as first-line therapy for couples with high fertilization and pregnancy rates and severe male factor infertility.
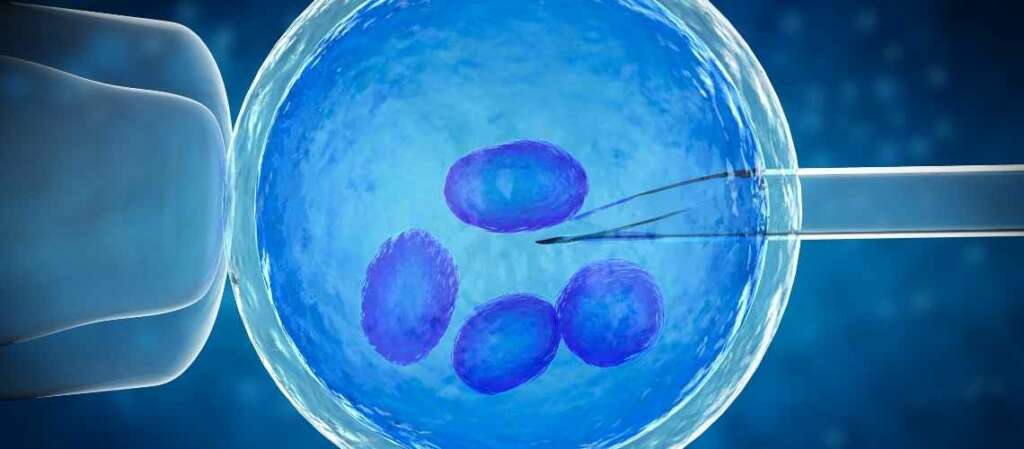
Intracytoplasmic sperm injection (ICSI) is an infertility treatment. It works by injecting live sperm into a person’s eggs in a laboratory. An embryo can be produced using this process (fertilized egg). An example of in vitro fertilization is ICSI. ICSI is most frequently used by medical practitioners when male infertility interferes with a person’s capacity to have children. (1)
Who can be a candidate for ICSI?
Your doctor may recommend ICSI,
- If your sperm count is too low.
- if your sperm are abnormally shaped (poor morphology) or not moving normally (poor motility).
- If you have had IVF and none or very few eggs have been fertilized.
- If you need to have sperm collected surgically from the testicles or epididymis (a narrow tube in the scrotum where sperm are stored and matured).
- If you are using frozen sperm that is not of the highest quality in your treatment, especially if it has been stored because your fertility is threatened, or after a surgical sperm collection.
- If you’re getting embryo testing for a genetic condition and sperm sticking to the outside of the eggs interferes with the results. (2)
How does ICSI work?
Your duration of treatment will be identical to that for IVF. The only difference is that a knowledgeable embryologist (embryo expert) will inject a single sperm into the egg rather than combining the sperm and eggs and allowing them to fertilize naturally.
This boosts the chances of conception since it avoids any potential obstacles the sperm would face when entering the egg.
How successful is an ICSI cycle?
ICSI is particularly effective at promoting sperm and egg fertilization. The woman’s age and if she has experienced any fertility problems are only two of the many other factors that can affect a healthy pregnancy, much like with IVF. Since ICSI success rates frequently resemble those of IVF, we do not disclose separate data about this procedure.
How safe is ICSI?
ICSI carries a little bit greater risk than some other reproductive therapies, including the chance that cleaning and injecting sperm will harm the eggs.
It has been suggested that the use of ICSI may also cause long-term health issues for newly born offspring. However, this cannot be proved either way until we have more conclusive evidence.
To avoid passing on a low sperm count to a boy, you might want to first think about genetic testing if you suspect this may apply to you. Before undergoing these tests, you should probably speak with the counselor at your clinic about all of the possible consequences.
Is ICSI more effective than other treatments?
ICSI using the husband’s spermatozoa demonstrated a greater incidence of fertilization compared to IVF with high insemination concentration (HIC)using the husband’s spermatozoa in patients with previously unsuccessful traditional IVF cycles that were unexplained (normal sperm count, motility, and morphology).
Comparing ICSI to traditional IVF with donor spermatozoa, patients with prior idiopathic failed HIC cycles had a higher incidence of fertilization with donor spermatozoa after ICSI. These findings demonstrated that, in the absence of any aberrant semen characteristics, ICSI produced a statistically higher overall number of fertilized oocytes when compared to traditional IVF or IVF with HIC.
What are the ethical considerations of ICSI?
The ethical considerations of Intracytoplasmic Sperm Injection (ICSI) within the IVF process demand careful deliberation. Firstly, the technique involves selecting a single sperm for injection into an egg. This selection raises genetic concerns. Specifically, there is a risk that the chosen sperm might carry undetected genetic abnormalities. Preimplantation genetic testing offers a mitigation strategy by screening for these potential issues before embryo implantation.
Moreover, ICSI increases the likelihood of multiple births. Such outcomes present significant health risks for both the mother and the infants involved. To address this, healthcare providers typically recommend strategies aimed at reducing the chances of multiple pregnancies. These include the transfer of a limited number of embryos during the IVF cycle.
Lastly, the allocation of resources becomes a critical ethical consideration. Given that ICSI is a more complex and costly procedure than traditional IVF, its application warrants a discussion on cost-effectiveness. It is crucial to prioritize its use for cases where the benefits to the couple are clear and significant. Together, these points underscore the importance of ethical mindfulness in the application of ICSI within IVF treatments.
Source:
1- Fishel, S., Aslam, I., Lisi, F., Rinaldi, L., Timson, J., Jacobson, M., … & Lisi, R. (2000). Should ICSI be the treatment of choice for all cases of in-vitro conception?. Human Reproduction, 15(6), 1278-1283.
2, and rest- https://www.hfea.gov.uk/treatments/explore-all-treatments/intracytoplasmic-sperm-injection-icsi/